Vaccination Discovered
Vaccination started much like variolation - and at first, the only major difference was that instead of using smallpox to infect patients, cowpox was used. This created a milder, localized infection that rarely spread between people and was overall less dangerous but still created immunity against smallpox. It was a great step forward for immunology and public health.
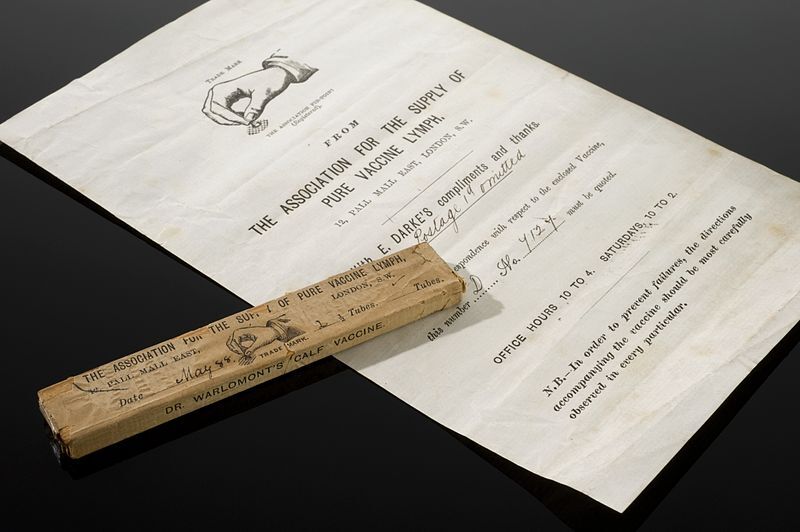
However, cowpox didn't spread the way smallpox did, and cowpox didn't occur in every part of the world, so a way to transport and maintain a supply of cowpox for vaccinations had to be developed. The two main methods were arm-to-arm transmission and mailing lymph (pus from sores) or scabs. Mailing lymph was unreliable. Extreme temperatures and the time it took for the lymph to travel could render it inactivated or otherwise degraded, and therefore useless for vaccination.
Arm-to-arm became the primary method for keeping viable stores of cowpox lymph. Most often children would be carriers on long journeys. A group of them would be taken to travel, with the children being vaccinated one by one over the course of the voyage to keep a supply going. This was also how supplies were spread when introduced to a new country, using those who had an infection from their vaccination to vaccinate others. It worked to an extent, but transmission chains were sometimes interrupted, and because cowpox didn't occur everywhere, if supplies ran dry, new supplies were needed.
Unfortunately, when coupled with unsanitary procedures, this arm-to-arm transmission led to the accidental spread of diseases like syphilis and leprosy. Because of the possible dangers of accidental transmission, and the difficulties with transmission in general, animals-- specifically cows-- started to be used more often as hosts for cowpox. Eventually, animal lymph became the primary supply for vaccines, and in several countries, dedicated vaccine farms were created for the express purpose of having a supply of vaccine lymph. (Esparza et. al, 2020)
Vaccination technique got better as the understanding of germ theory improved. New ways of injecting vaccines into a person were invented, and eventually, the material needed to make vaccines could be produced in a lab without animal or human hosts. Quality controls and standardization improved as well, leading to better and more effective vaccines and enabling hope for a world without fear of smallpox.
Though Edward Jenner, scientists, and doctors of the time didn't understand how vaccination worked, we now have a much more sophisticated idea of how the immune system defends against pathogens and creates immunity.
When a new pathogen (disease-causing organism) enters the body, it can multiply and cause an infection, which in turn results in an illness. This most often happens when your body hasn't yet developed a defense for that pathogen and cannot provide an adequate defense against it in time. Usually, when you get sick, your immune system sends T-cells and B-cells (special immune cells) to the infection. The body creates antibodies against the pathogen and "memory" T-cells remember that antibody so if the immune system encounters that pathogen again, it can mobilize much faster, create antibodies, and attack the pathogen before it can multiply enough to cause an infection.
Vaccines take advantage of this and mimic infection by giving the immune system part of a pathogen, enough to cause a reaction but not enough to cause noticeable side effects. That infection, though small, still creates memory T-cells that are stored by the immune system and can then be mobilized if the body ever comes into contact with the full pathogen.
(How do vaccines work?, WHO), (Understanding how vaccines work, CDC)